On June 19, the Department of Labor (DOL) issued a final rule allowing employers, regardless of size, to offer health insurance through an Association Health Plan (AHP). The final rule loosened the definition of “employer” under the Employee Retirement Income Security Act (ERISA) and thereby permitted the bypassing of certain regulatory requirements. The rule focuses on benefiting small employers and self-employed workers by allowing them to offer plans through an association with other employers that would be treated like large group health plans. That is, such plans would not need to comply with rules applicable to individual or small group plans.
An AHP may be formed by satisfying the so-called commonality of interest test, which can focus either on geography or industry. Regarding the former, different employers who nevertheless share the same trade, industry or profession—regardless of location—may form an AHP. As to the latter, employers in the same geographic area—regardless of industry—may likewise form an AHP. The relevant geographic area may be a greater metropolitan region that falls within the boundaries of more than one state. Under the previous framework, the association needed to satisfy both the industry and the geographic requirements.

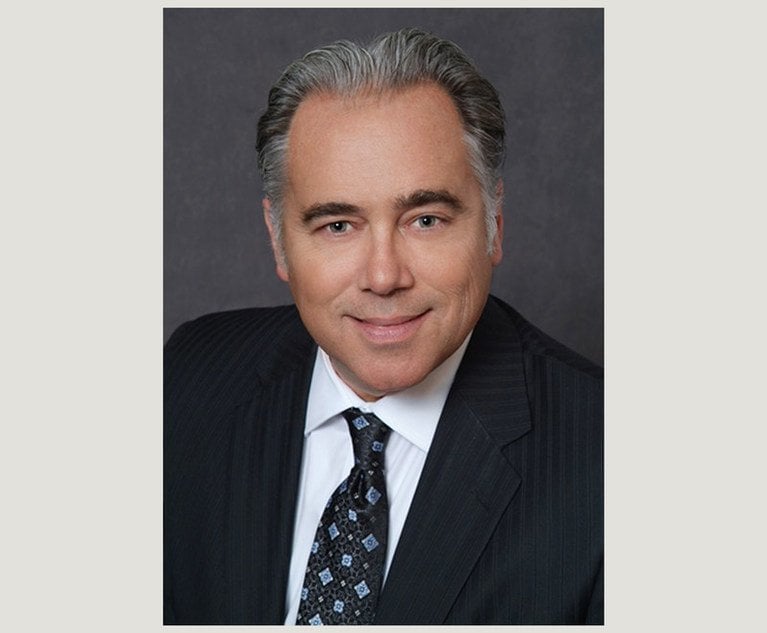
 Vasilios “Bill” Kalogredis.
Vasilios “Bill” Kalogredis.